A “One Health” Approach to AMR
This is part of a communication series to health leaders in GHM’s partner countries. (sent February, 2022)
Fostering international cooperation on antimicrobial resistance (AMR)
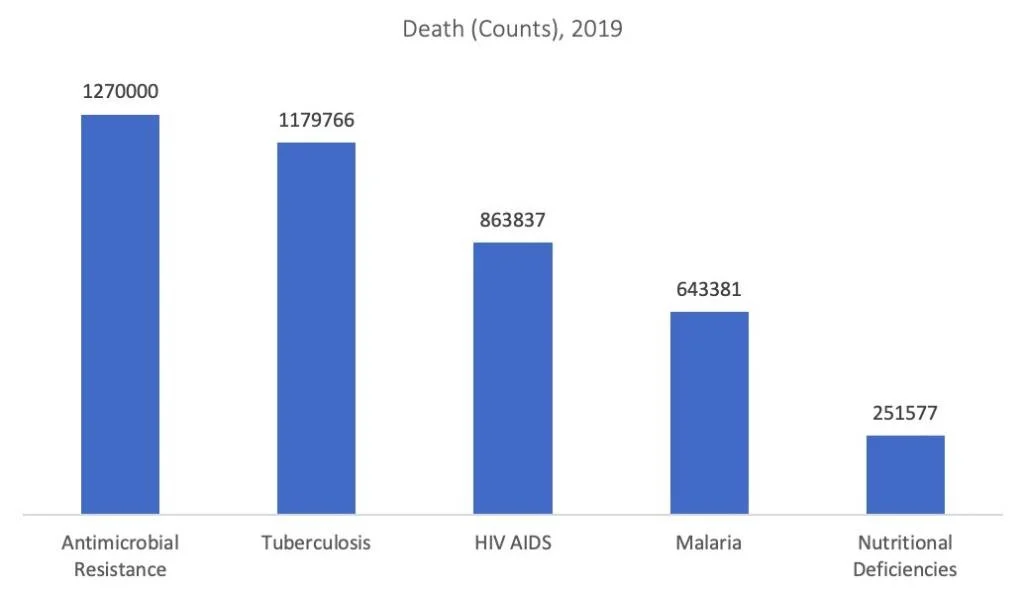
Antimicrobial resistance (AMR) is a major threat to human health globally, according to a study published in Lancet in January 2022 - the most comprehensive estimates of AMR burden to date. The study highlights that AMR has become a leading cause of death worldwide, killing about 3,500 people every day. The study estimates 127M deaths attributed to AMR and 495M associated with AMR in 2019.
Deaths Due to Different Causes, 2019
* Source: Lancet study and IHME GBD tool
Bacterial antimicrobial resistance (AMR) occurs when changes in bacteria cause the drugs used to treat infections to become less effective.
The UK Review on Antimicrobial Resistance asserted that AMR could kill 10 million people per year by 2050. Antimicrobial resistance (AMR) has been referred to as “a ticking time bomb” for the world, and notably for India.
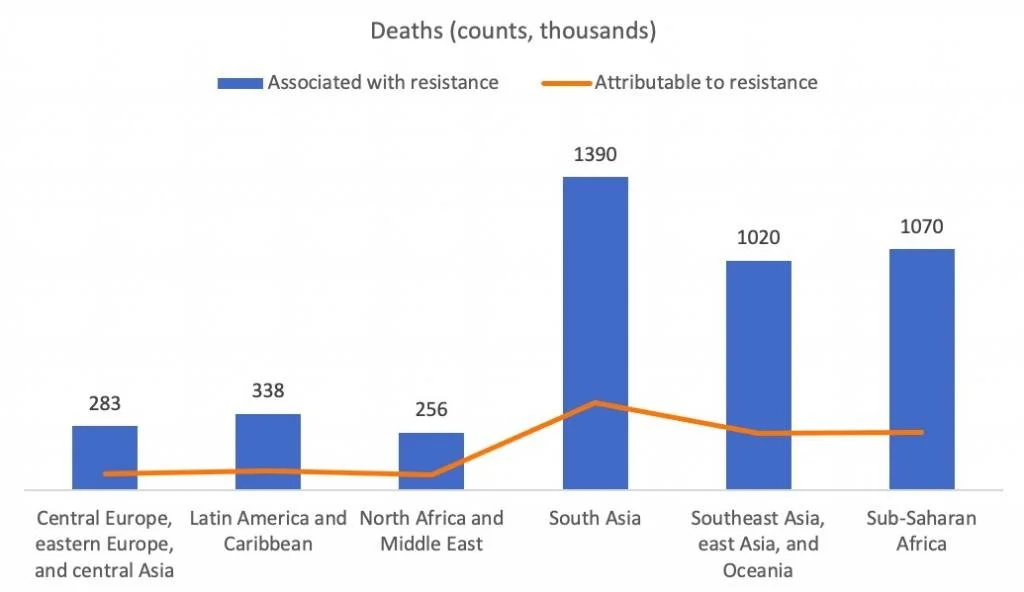
Deaths Associated and Attributable to Bacterial AMR
*Source: Lancet study
Covid-19 Impact on AMR
While AMR, a contagion of deadly bacteria becoming resistant to antibiotics, has been decades in the making and “waiting in the wings,” COVID-19 appears to have exacerbated the AMR challenge.
Findings from a recent study from the Pew Charitable Trusts are summarized below:
A majority of COVID-19 hospital admissions led to one or more antibiotics being given to patients. Over half of the COVID-19 hospital admissions captured in this study (52%) resulted in at least one antibiotic prescription, with 36% of admissions resulting in a patient being prescribed multiple antibiotics during hospitalization.
Compared to the number of hospitalized COVID-19 patients who received antibiotics, far fewer patients admitted for COVID-19 had common bacterial infections. Only 20% of those admitted with the virus were diagnosed with suspected or confirmed bacterial pneumonia, and 9% were diagnosed with a community acquired urinary tract infection.
In most cases, antibiotics were given to COVID-19 patients prior to confirmation of a bacterial infection. In 96% of admissions for patients diagnosed with COVID-19 in which an antibiotic was prescribed, the patient received the first antibiotic at admission or within the first 48 hours of hospitalization. It typically takes at least 48 hours to confirm a bacterial infection, so it appears that physicians frequently prescribed antibiotics empirically, i.e., before confirmation of a known bacterial infection. The findings strongly suggest that overprescribing of antibiotics occurred during the first six months of the pandemic.”
Finding a Balance
It is critical to ensure that solutions avoid limiting access to antibiotics for those who need it. While reducing misuse and overuse is central to addressing the problem of antibiotic resistance, it is estimated that more people die from no access or delayed access to antibiotics than from antibiotic resistance.
During the COVID-19 pandemic, attention and resources have shifted away from AMR management programs for epidemiologists, antimicrobial stewardship experts, and infectious disease doctors. As professionals were stretched thin by urgent new priorities and rapidly evolving data, many stewardship practices were deprioritized. Also, in the fight to help acutely ill patients, more medical devices such as ventilators, central lines, and catheters created secondary infections with increased risk for hospital-acquired infections.
Lessons for Global Health Leaders
Global scope. AMR must be seen as a global issue, which needs a globally coherent plan with a globally governed “One Health*” approach. The One Health approach to AMR includes coordination of human, animal, plant and environmental policies. Like, COVID-19, AMR is a complex problem that transcends borders and cannot be tackled by a single country or international agency.
UN Integrated approach. The UN secretary general convened the Tripartite of WHO, FAO and the OIE to form an Interagency Coordination Group (IACG) on AMR to provide guidance on what global actions are needed and to finalize a proposed Global Framework for the Development and Stewardship to Combat AMR.
Financing. The Global Fund to Fight AIDS, Tuberculosis and Malaria has an opportunity at its 2022 20th anniversary meeting to review its fundamental purpose to invest in programs to end the infectious diseases that cause the greatest burden, especially in low- and middle-income countries (Lancet 1/22/22).
Asante/Gracias/Misaotra/Merci/Thank you for your leadership in helping to tackle the top infectious diseases in the world, including AMR!
Rob Thames, FACHE, FHFMA, Director, GHAP (Global Health Administration Partners)
Update on the Race between the Virus, Vaccinations … and Variants
Vaccinations – According to the Bloomberg COVID-19 Vaccine Tracker as of 31 January, 2022:
A shot in the arm: Over 10.1 Billion doses have been given in 184 countries. The current rate is over 32.4M doses per day; over one-fifth of this (~7.4M) are people getting a first shot - at this rate, it would take ~5 months to cover 75% of the population. Because of the variants, it is believed that a higher rate of coverage is needed to achieve a herd immunity effect.
Countries: Globally, 129 doses have been given for every 100 people.
Virus – Globally, according to the JohnsHopkins COVID-19 Tracker as of 31 January 2022, the reported COVID-19 infection count is:
5.67M deaths – this is nearly the population of Denmark. Reality? A recent study by the Economist using machine learning estimated as many as 17 million people world-wide, more than three times the reported number, had died of Covid-19;
375 million COVID-19 cases have been reported – while experts concur that the actual number of people infected is a multiple of this reported number, it is still larger than the population of the United States;
Check out the February 4 blog on this website for a COVID-19 update on GHM Partner countries, thanks to Lon Kightlinger, epidemiologist and GHM Board member.